Symptoms and consequences of anodyspareunia in gay and bisexual men treated for prostate cancer
This is a study that I will present at the 2022 International Academy of Sex Research annual scientific conference.
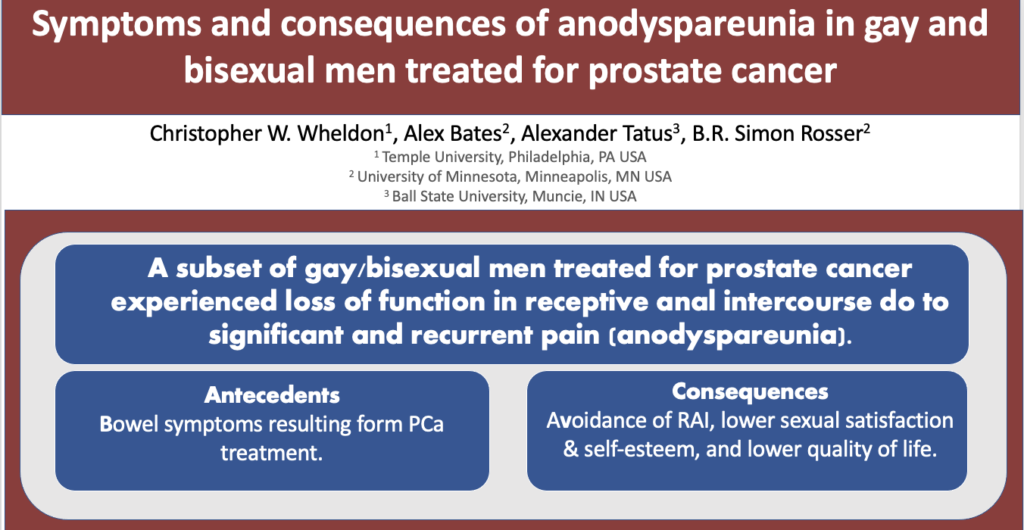
Introduction: Sexual dysfunction is a common adverse outcome of prostate cancer (PCa) treatment. In prostate cancer research, sexual dysfunction is based on heteronormative assumptions of sex (e.g., erections firm enough for vaginal intercourse); therefore, current evidence to inform clinical practice is not responsive to the needs of gay and bisexual men (GBM). In addition to erectile dysfunction, GBM describe significant distress related to the loss of pleasure and the experience of pain during receptive anal intercourse (RAI). Anodyspareunia—defined as recurrent or persistent pain experienced during RAI—is an important attribute of sexual function for GBM adversely impacted by PCa treatment. Anodyspareunia is conceptually related to Genito-Pelvic Pain/Penetration Disorders (GPPPD). It is estimated that 10-14% of GBM in the general population experience anodyspareunia. The purpose of this study was to: (1) describe clinical symptoms of painful receptive anal intercourse in GBM following PCa treatment; (2) to estimate the prevalence of anodyspareunia; and (3) to identify clinical and psychosocial correlates.
Methods: Data were from the Restore-2 study, a longitudinal online survey of 401 GBM treated for PCa in the U.S. or Canada. The analytic sample included only those participants who attempted RAI during/since their PCa treatment (N=195). Participants were asked about the frequency of pain during RAI since completing PCa treatment, in addition to the duration, intensity, and distress resulting from the pain. Anodyspareunia was operationalized as moderate to severe pain during RAI for six months or longer that resulted in mild to severe distress. Logistic regression was used to identify bivariate correlates.
Results: Overall, 82 (42.1%) participants reported pain during RAI since completing PCa treatment. Among this group, 45.1% experienced painful sometimes or frequently and 63.0% indicated that periods of painful RAI lasted at least six months. The intensity of pain at its worst was moderate to very severe for 79.0% of participants. The experience of pain was at least mildly distressing for 63.5% of participants. For over a third (33.4%), painful RAI worsened after prostate cancer treatment. For most, the enjoyment of RAI was decreased due to pain (58.6%). Overall, 15.4% were classified as meeting criteria for anodyspareunia. Being single vs. married/partnered (OR=2.34; 95% CI: 1.03-5.31) and having a higher prostate specific antigen score (OR=1.02; 95% CI: 0.99, 1.05) were associated with higher odds of anodyspareunia. Better bowel function (OR=0.96; 95% CI: 0.93, 0.99) and higher sexual self-esteem (OR=0.90; 95% CI: 0.84, 0.96) were negatively associated with anodyspareunia. Treatment type (radiation vs. surgery only) was not associated with anodyspareunia.
Conclusions: Approximately 1 in 7 GBM PCa patients described symptoms of anodyspareunia with clinical criteria similar to other GPPPD. Anodyspareunia was a problem independent of PCa treatment. Culturally responsive cancer care for GBM should address changes to RAI and its potential impact on quality of life. Future research needs to evaluate protocols for sexual rehabilitation of anodyspareunia.